Women’s health conversations have come a long way, but there’s still a massive gap between what gets discussed openly and what actually affects millions of women every day. While breast cancer awareness and prenatal care dominate public health campaigns, countless other issues remain frustratingly invisible. These aren’t rare conditions or minor inconveniences—they’re real problems that impact work performance, relationships, mental health, and quality of life.
Women’s health conversations have come a long way, but there’s still a massive gap between what gets discussed openly and what actually affects millions of women every day. While breast cancer awareness and prenatal care dominate public health campaigns, countless other issues remain frustratingly invisible. These aren’t rare conditions or minor inconveniences—they’re real problems that impact work performance, relationships, mental health, and quality of life.
The silence around certain women’s health topics isn’t just awkward. It creates a situation where women suffer unnecessarily, often assuming their experiences are abnormal or that no solutions exist. Breaking down these barriers means having honest conversations about the full range of health concerns women face throughout their lives.
The Menstrual Taboo That Won’t Quit
Periods are a biological reality for roughly half the population, yet they remain weirdly controversial to discuss. Most women have dealt with a cycle that decided to show up at the worst possible time—vacations, weddings, important exams, or athletic competitions. The frustration of having your body’s schedule clash with your life plans is something nearly every woman can relate to, but solutions rarely get mentioned outside of doctor’s offices.
Here’s what many women don’t realize: medical options exist for managing menstrual timing when life events don’t cooperate with biology. For women facing significant disruptions, period delay tablets prescribed through legitimate medical channels can provide the flexibility needed for important occasions. This isn’t about eliminating periods entirely or treating normal menstruation as a disease—it’s about acknowledging that sometimes, women need options that work with their lives rather than against them.
The reluctance to discuss period management stems partly from outdated attitudes that women should simply endure whatever their cycle brings. That mindset doesn’t hold up in today’s world, where women compete in high-level athletics, travel frequently for work, and plan significant life events that shouldn’t be derailed by bad timing.
Painful Sex Nobody Wants to Mention
Dyspareunia—painful intercourse—affects somewhere between 10% and 20% of women at some point in their lives. Those numbers are probably low because many women never report it, assuming the problem is their fault or just something to tolerate. The causes range from medical conditions that need treatment to hormonal changes, stress, or relationship dynamics that need addressing.
The problem is that when women do try to discuss painful sex, they often encounter dismissive responses or vague suggestions to “relax more.” This leaves women stuck in a frustrating cycle of discomfort, avoiding intimacy, and feeling broken. Real solutions exist depending on the underlying cause—medical treatments, pelvic floor therapy, hormone adjustments, or working with specialists who actually take the concern seriously.
What makes this particularly challenging is that painful sex doesn’t just affect physical health. It damages relationships, creates anxiety around intimacy, and chips away at self-esteem. Yet it remains one of those topics women whisper about to close friends rather than demanding proper medical attention.
The Postpartum Reality Check
Pregnancy and childbirth get plenty of attention, but the postpartum period? That’s where the support system tends to collapse. Women are expected to bounce back quickly while dealing with hormonal chaos, sleep deprivation, physical recovery, and the demands of a newborn. The cheerful narrative about motherhood being purely joyful doesn’t leave much room for the reality many women face.
Postpartum depression and anxiety affect roughly one in seven women, but many suffer silently because admitting to negative feelings about new motherhood feels forbidden. Physical issues also get brushed aside—incontinence, ongoing pain, or complications from delivery—as though these are just normal sacrifices mothers should accept. The “your body will never be the same” attitude discourages women from seeking treatment for problems that could actually be resolved.
Beyond depression and physical recovery, postpartum rage is only recently getting recognition as a legitimate response to hormonal shifts and stress. Women experiencing intense anger or irritability often feel intense shame, worried they’re bad mothers rather than recognizing this as a symptom that deserves attention.
Perimenopause: The Long Goodbye Nobody Prepared You For
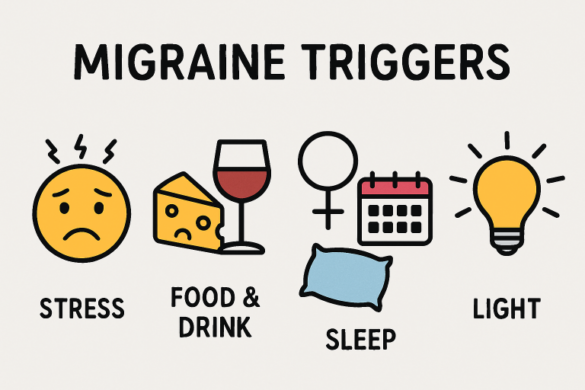
Most women know menopause exists, but perimenopause—the years-long transition beforehand—catches many completely off guard. It can start in a woman’s 40s or even late 30s, bringing irregular periods, mood swings, sleep problems, and a host of other symptoms that get dismissed as stress or aging.
The problem is that symptoms are often attributed to everything else before anyone considers hormonal changes. A woman experiencing anxiety, brain fog, or irregular cycles might go years without proper diagnosis simply because perimenopause doesn’t fit the narrow “older woman with hot flashes” stereotype most people have in mind.
This transition can last a decade, affecting women during peak career years and active family life. Yet comprehensive information and treatment options remain frustratingly hard to access. Many doctors still aren’t well-versed in managing perimenopause symptoms, leaving women to figure things out through online forums and trial and error.
Moving the Conversation Forward
What connects all of these issues? Nobody talks about them. When women don’t hear others discussing these problems, they assume something’s wrong with them personally rather than recognizing widespread health concerns. Medical research stays underfunded because the issues seem rare when they’re actually common. Treatment options remain limited because demand stays artificially low.
This pattern needs to break somewhere. Women need straight answers about what’s happening to their bodies without being told to just deal with it. Doctors need better training that goes beyond reproductive health basics. And honestly, society needs to get over the discomfort of discussing women’s actual health experiences rather than the sanitized versions that make everyone comfortable.
The shift happens when women refuse to stay quiet about what they’re going through. The more these conversations happen—between friends, with doctors, in public spaces—the harder it becomes to pretend these are fringe issues that don’t need attention or resources. Change won’t happen overnight, but it starts with refusing to accept inadequate answers to legitimate health concerns.