Understanding Collaborative Care
Collaborative mental health care is fundamentally changing the paradigm of support for those facing mental health challenges. By bringing behavioral health services into primary care environments, patients experience a more seamless and connected journey to wellness. This means that mental health services are no longer isolated, but are instead coordinated and easily accessible within familiar healthcare settings. If you’re looking for integrated support, you can learn more about these mental health services that are at the forefront of this approach.
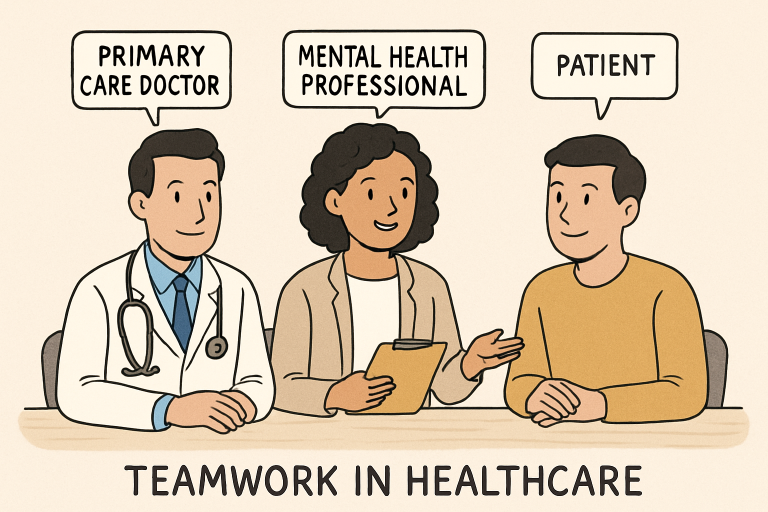
The collaborative model is driven by a team-based approach in which key professionals—including primary care providers (PCPs), behavioral health managers, and psychiatric consultants—work closely together. Their shared goal is to create cohesive, tailored treatment plans that address the physical, psychological, and social needs of each patient. This multidisciplinary structure ensures that no aspect of a person’s health is neglected.
Unlike traditional models, which treat mental and physical health separately, collaborative care fosters synergy between providers. This results in better communication, continuity of care, and ultimately, more effective interventions. By prioritizing holistic well-being, collaborative care is paving the way for a more compassionate and responsive healthcare system.
The National Alliance on Mental Illness (NAMI) further notes that such integration supports early detection and quicker intervention, especially important for individuals dealing with multiple or complex health issues.
Improved Patient Outcomes
Multiple studies consistently demonstrate that collaborative care models outperform traditional treatment approaches, especially for patients with depression and anxiety. According to a Cochrane review published in the Cochrane Database of Systematic Reviews, collaborative care is associated with significantly higher rates of symptom reduction and treatment completion than usual care.
Roughly half of all patients experience a 50% or greater reduction in their mental health symptoms, with many seeing improvement in less than four months. These positive outcomes have been observed across various populations, regardless of age, socioeconomic status, or the mode of service delivery (in-person or telehealth). Such broad-based effectiveness highlights the potential for collaborative care to serve as a gold standard in mental health treatment.
Enhanced Access to Care
One of the most significant advantages of collaborative care is improved access to mental health services, particularly in underserved or rural regions. By embedding behavioral health professionals within primary care offices, patients can seek mental health support in settings that are convenient and familiar, thereby reducing the need for referrals to specialized clinics that may have long waitlists or be geographically inaccessible.
Innovative policies are driving this integration forward. For example, programs like Colorado’s Medicaid initiative have begun reimbursing providers for the additional time and effort required in collaborative models, thereby helping to bridge care gaps for vulnerable populations.
Cost-Effectiveness
Beyond the clear clinical benefits, collaborative care also translates to cost savings for both patients and the healthcare system. Evidence suggests that adopting this model can lead to a reduction in healthcare spending of up to 13% compared to traditional approaches, primarily due to a decrease in emergency room visits and hospitalizations.
By focusing on prevention and early intervention, collaborative care not only addresses mental health needs more efficiently but also reduces the burden on acute care facilities. As a result, health systems can allocate resources more effectively, expanding access while controlling expenses.
Addressing Health Disparities
Collaborative care is playing a pivotal role in decreasing health disparities, especially among racial and ethnic minority groups who have historically faced barriers to mental health treatment. According to findings from the National Institute of Mental Health, implementing such models significantly reduces symptoms of conditions like PTSD within these populations.
Providing culturally attuned, coordinated care helps break down stigma and logistical hurdles, making mental health services more equitable. By meeting people where they are, collaborative care nurtures trust and long-term engagement in the healing process.
Integration of Technology
Modern technology is advancing collaborative care, making it even more accessible and user-friendly. A notable example is Illinois’s partnership with Google in creating the Beacon mental health services portal for youth. This digital platform streamlines the intake and coordination process for caregivers, enabling them to upload essential information just once and avoid redundancies.
With the rise of telehealth and data integration tools, patients and providers can communicate more efficiently, track progress, and adjust care plans in real-time. Such technological advancements are breaking geographical and administrative barriers in mental healthcare delivery.
Challenges and Considerations
Despite its many strengths, collaborative care does face notable challenges. Successfully implementing this model demands robust training for primary care providers, ongoing funding to support integration, and seamless communication pathways among team members. Additionally, adapting collaborative care to fit varying healthcare settings—such as large hospital networks versus small clinics—requires flexibility and careful planning.
Addressing these challenges is essential for sustaining the progress collaborative care has already made. Policymakers, health administrators, and practitioners must work together to establish workflows and incentives that support effective, holistic mental health care.
Conclusion
The collaborative care model is revolutionizing how mental health is addressed within the broader healthcare system. With its focus on integration, teamwork, and patient-centeredness, it delivers superior outcomes, expands access, and reduces disparities and costs. As the healthcare landscape continues to evolve, collaborative mental health care is poised to become the standard for effective, equitable treatment—ultimately paving the way for healthier, more empowered communities.